If Safety Is Your Yardstick, Measuring Culture from the Top Down Must Be a Priority
During the past decade, those most involved in the patient safety movement have come to realize that preventing catastrophic events—or, for that matter, any preventable patient harm—requires more than changing systems and implementing best practices. It also requires a change in our mindset about patient safety, and a change in the underlying culture in which healthcare is provided, assessed, and improved.
In fact, one of the most significant predictors of success with keeping patients safe is the state of an organization’s culture.1 How open are people to reporting risk, near misses, and errors? Do people regard near misses as system failures that reveal potential danger or evidence of success since potential harm was avoided? How receptive are the leaders to hearing about problems that affect patient safety? Is it just by chance that more serious mistakes don’t happen? The answers to these questions and more about the culture cannot be found in a single individual. The entire organization, from the board to the front-line workers, needs to be surveyed to establish a baseline that describes the current culture upon which strategies for improvement can be determined and repeat measurements can demonstrate change.1
An organization’s “culture” can be found in the pattern of shared basic assumptions about the organization’s values (what is important), beliefs (how things work), and behaviors (the way we do things) that have been taught to the workforce in both explicit and implicit ways.2 Thus, the culture encompasses both the observable customs, behavioral norms, stories, and rites that occur in an organization as well as the unobservable assumptions, values, beliefs, and ideas shared by groups.
In several 2005 and 2006 newsletters,3-6 we described many of the attributes of a culture of safety. Building upon this work, nurse leaders who attended the second annual Nursing Leadership Congress in September 2006 identified the domains of a culture of safety that should be measured.7
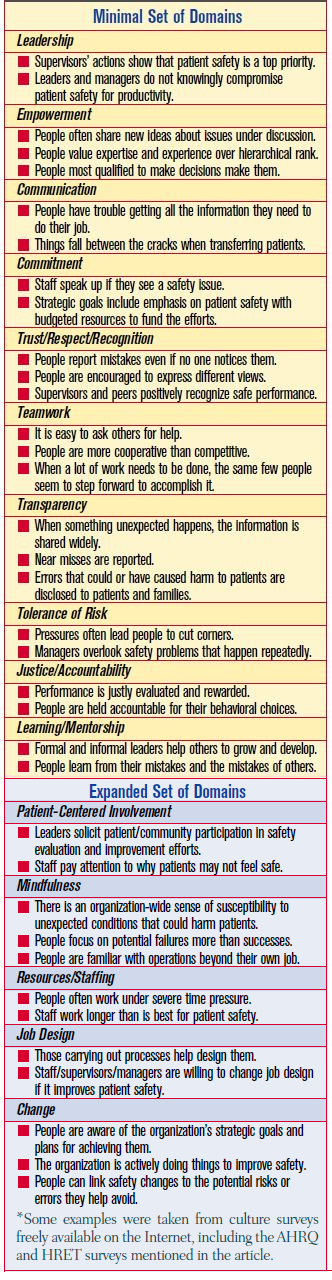
The domains were divided into a minimal set that should be addressed in all culture measurement, and an expanded set for more in-depth culture measurement. Table 1 provides a list of these domains and examples of assessment items that could be included to measure each domain.
The most common means of measuring organizational culture is to survey an adequate sampling of staff. Two examples of validated survey tools can be found on the Web sites of the Agency for Health- care Research and Quality (AHRQ) (www.ahrq.gov/QUAL/hospculture/) and the Health Research and Education Trust (HRET) (www.hret.org/hret/programs/saq.html). These tools, which were both launched in 2004, can be downloaded free of charge. In March 2006, ARHQ also began gathering eligible survey data into a central repository, which may become the first nationally available comparative database on organizational culture.
In addition to staff surveys, there are other ways to add to the pool of knowledge about the culture, as described below.
Patient surveys. Surveys can be used to determine the perceptions that patients and the community have about the organizational culture.
New hire interviews. During the first few months, new staff can be asked: 1) Are we doing things differently than what we said? 2) When you first joined the organization, what details struck you? and 3) Is there anything that makes you want to leave? Answers to these questions can help pinpoint cultural issues, particularly those in conflict with the organization’s espoused values.
Rounding. Patient safety rounds can be used as a forum to learn more about the culture, particularly if standard queries are included in the script used for interaction with staff and patients.
Focus groups. Small groups can gather to discuss the organization’s progress toward reaching a culture of safety. Clues can be gathered about cultural domains that should be targeted by asking staff: What would you tell a new colleague about what they need to know to get their job done?
Exit interviews. Staff turnover rates and information gleaned during exit interviews can help uncover undesirable cultural elements that exist.
Performance evaluations. Aggregate data on cultural domains used to measure the performance of all staff (e.g., teamwork, communication, respect, transparency) can be gathered.
The aggregate information obtained about the culture should be used to perform a gap analysis between the current culture and the ideal culture to identify opportunities for improvement. Comparing data from various large groups can also provide important information. For example, comparisons can be made between the perceptions of: board members and the executive team; the executive team and management; management and staff; new staff and experienced staff; nurses and pharmacists; patients and providers; and so on. Differences in perceptions of the culture among specific groups can point out problems that may not be detected by analysis of the aggregate data alone.
Findings from measuring the culture should be shared with all staff in the organization, and its meaning should be clearly articulated. Feedback about how to move in the direction that best supports patient safety should be sought throughout the organization. The more you ask for feedback and act on it, the faster change will occur.1 As an added bonus, the surveying process itself can help an organization articulate the most important aspects of the desired culture, and the actions taken in response to survey findings can firmly establish the organization’s commitment to a culture of safety. Culture data should also be used to demonstrate improvement in key safety culture domains over time. However, the same tools should be used to measure the same groups so that internal comparisons are valid. New measures can be introduced as desired, but a core group of key measures should remain unchanged.
Laying a foundation for a culture of safety takes time, commitment, and practice within the domains described in Table 1. But simply checking off the domains is no indication of an organization’s progress toward a culture of safety. The organization may have an event reporting program, a reasonably just culture, and a fair amount of measurement and team-work. It may have succeeded in implementing some important safety measures. However, as Reason notes, “assembling the parts of a machine is not the same thing as making it work.”(8) It is not enough to possess some of the elements of a culture of safety. A total transformation in the way we perceive and react to risks that threaten the safety of patients is needed. Measuring the culture builds the groundwork for this transformation.
References
- Smetzer J, Navarra MB. Measuring change: a key component of building a culture of safety. Nursing Economics 2007; 25(1):49-51.
- Senge P, Kleiner A, Roberts C, et al. The dance of change. 1999; Currency:NY, NY.
- ISMP Medication Safety Alert! High-reliability organizations (HROs): what they know that we don’t, part I. 2005; 10(14):1-2.
- ISMP Medication Safety Alert! High-reliability organizations (HROs): what they know that we don’t, part II. 2005; 10(15):1-3.
- ISMP Medication Safety Alert! Safety requires a state of mindfulness, part I. 2006; 11(5):1-2.
- ISMP Medication Safety Alert! Safety requires a state of mindfulness, part II. 2006; 11(6):1-2.
- Nursing Leadership Congress. Building the foundation for a culture of safety, 2006 proceedings. Alpharetta, GA: McKesson Corporation; 2007.
- Reason J. Managing the risks of organizational accidents. Hants, England: Ashgate Publishing Ltd; 1997 (page 219)
