Students Have a Key Role in a Culture of Safety: Analysis of Student-Associated Medication Incidents
Undergraduate and postgraduate students in healthcare fields are attempting to develop the skills required to deliver safe and effective patient care as future practitioners. As part of their training, most students are exposed to a variety of practice environments and direct patient care experiences to help prepare them for their eventual careers. This hands-on experience places students in a position to be involved in medication errors or to catch and prevent errors before they reach patients.
More than a decade ago, ISMP published an analysis of medication errors involving student nurses that had been reported to the ISMP National Medication Errors Reporting Program (ISMP MERP) and the Pennsylvania Patient Safety Reporting System (PA-PSRS).1 Based on that analysis, some student-related errors were similar in origin to those that seasoned licensed healthcare professionals make, such as misidentifying medications due to look-alike labels and packages, or making a mental slip when distracted. Other errors stemmed from system problems and practice issues that were unique to environments where students and hospital staff are simultaneously caring for patients. Staff and students assigned to the same patient is a prime example of how errors can happen. While dual assignments are necessary, communication breakdowns regarding who will administer the prescribed medications to patients, what medications have been administered, and which medications should be held, have resulted in dose omissions and extra doses.
In 2016, an analysis of healthcare student errors reported to the Pennsylvania Patient Safety Authority through PA-PSRS was published, which identified insulin, opioids, and anticoagulants as the most common high-alert medications involved in student-related errors, although less than 1% of the errors resulted in patient harm.2 Most of the errors involved nursing students, during which an instructor or preceptor was involved or present approximately a quarter of the time. More than two-thirds of the errors occurred during peak academic periods—February through April and September through November.
Earlier this year, a lack of Canadian literature describing the impact of healthcare students on medication safety prompted our sister organization, ISMP Canada, to analyze 616 student-associated medication incidents reported to three of its medication incident reporting databases and the Canadian National System for Incident Reporting (NSIR) between April 2013 and March 2017.3 The following describes the main themes identified in the analysis, along with examples illustrating the students’ role in a culture of safety.
Qualitative Findings
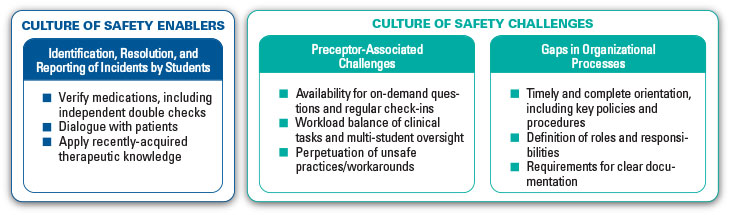
Student-associated medication incidents involved multiple disciplines and occurred in a wide variety of healthcare settings. When examining the events from a culture of safety perspective, analysts identified both safety enablers and challenges (Figure 1). Within these two groups, there were three main themes, each with multiple subthemes.
CULTURE OF SAFETY ENABLERS
THEME: Identification, Resolution, and Reporting of Incidents by Students
Students were active in recognizing, resolving, and reporting medication incidents made by other members of the team. In 263 (43%) of the 616 reports, students identified and reported the error. The current practice of teaching medication safety principles to healthcare students supports a culture of safety, which may have provided a basis for students to identify and report incidents. Two key activities that enabled students to identify incidents were participation in medication verification and dialogue with patients.
Incident Example 1:
DEPO-MEDROL (methylPREDNISolone acetate) labeled “For IM, Intrasynovial and Soft Tissue Injection Only, Not for IV Use” was mistakenly dispensed instead of SOLU-MEDROL (methylPREDNISolone sodium succinate) intended for intravenous (IV) administration. Following the correct procedure for medication checks, a nursing student recognized the error and brought it to the preceptor’s attention before it was given.
Incident Example 2:
A prescription for VALTREX (valACYclovir) 500 mg twice daily for 6 days was received and processed at a community pharmacy. During patient counseling, a pharmacy student learned that the medication had been prescribed to treat a cold sore. The recommended regimen for this indication (Valtrex 2 g every 12 hours for 1 day) was suggested to, and accepted by, the prescriber.
PRACTICE TIP #1:
Students bring a new perspective to the medication-use system and should be encouraged to question, identify, and report errors/gaps.
CULTURE OF SAFETY CHALLENGES
THEME: Preceptor-Associated Challenges
The value of effective oversight and support from preceptors during students’ rotations cannot be overstated. The availability of preceptors for both on-demand questions and regular check-ins is a critical component of a safe training environment. Factors contributing to inadequate oversight include high preceptor workload (e.g., preceptorship of multiple students, preceptorship of students in multiple locations, concurrent clinical demands) and lack of engagement on the part of the preceptor. Lack of preceptor oversight has previously been cited as a contributing factor associated with medication errors.4
Incident Example 3:
A nursing student contacted the instructor to observe measurement and administration of insulin. They realized that only a small amount of insulin remained in the vial, which was not enough for the patient’s dose. The instructor asked the student to find another vial, then left to help other students. The instructor did not return. The student eventually had to ask other nursing staff for assistance, and the insulin was administered late.
PRACTICE TIP #2:
Be sure that the preceptor’s workload accounts for the level of supervision each student needs to optimize his/her learning in a safe environment.
THEME: Gaps in Organizational Processes
Incident reports highlighted situations in which tasks were delegated to students before they were adequately oriented and prepared to perform them. Like other studies,1,2 error-prone processes such as simultaneous preparation of medications for multiple patients contributed to several of the incidents. Other reports described students not following organizational policies and procedures, noting that the students may not have been aware of them and/or staff may not have been following them to set a good example.
Incident Example 4:
A healthcare practitioner asked a medical student to retrieve a syringe of midazolam to administer IV in preparation for an epidural injection, while pointing to the supply area where the syringe was lying. The student handed the practitioner a syringe containing the neuromuscular blocking agent, rocuronium, instead. The drug was administered, and the patient became paralyzed and required intubation.
Incident Example 5:
In an outpatient pharmacy, a pharmacy student was asked to refill the metFORMIN bin in a robotic prescription dispensing system, a process which involved selecting and scanning the bottle label prior to pouring the tablets into the machine. With the aim of improving efficiency, the student picked up 4 bottles of medication but scanned the label of only 1 bottle 4 times instead of scanning each individually. The scanned bottle contained metFORMIN, but one of the other bottles selected contained acetaminophen with codeine tablets; both products were round, white tablets. As a result, two different medications were added to the same compartment of the robotic prescription dispensing system.
PRACTICE TIP #3:
Review organizational challenges impacting students at your facility to identify opportunities to improve the culture of safety.
Conclusion
The themes identified in this analysis illustrate the positive contribution students can make to medication safety, the importance of preceptor oversight, and the need for robust organizational processes that are followed by students and staff. While the inexperience of students has been described as a factor contributing to medication incidents,1,2 there are also positive aspects to having students in real-world healthcare settings. For example, they bring a unique perspective and question processes that could allow opportunities for error. Students can play a key role in a culture of safety if organizational processes and educational programs focus on optimizing that role. It is paramount that future practitioners are trained in environments that support safe medication use and that allow them to utilize their knowledge to reduce opportunities for errors.
References
- ISMP. Error-prone conditions that lead to student nurse-related errors. ISMP Medication Safety Alert! 2007;12(21):1-2.
- Hess L, Gaunt MJ, Grissinger M. Medication errors involving healthcare students. Pa Patient Saf Advis. 2016;13(1):18-23.
- ISMP Canada. Students have a key role in a culture of safety: a multi-incident analysis of student-associated medication incidents. ISMP Canada Safety Bulletin. 2018;18(2):1-3.
- Reid-Searl K, Moxham L, Happell B. Enhancing patient safety: the importance of direct supervision for avoiding medication errors and near misses by undergraduate nursing students. Int J Nurs Pract. 2010;16(3):225-32.
ISMP thanks ISMP Canada for sharing its analysis and report on this topic.3
