Administration of Concentrated Potassium Chloride for Injection During a Code: Still Deadly!
Problem: Decades ago, ISMP became aware of multiple patient injuries and fatalities associated with the accidental intravenous (IV) administration of concentrated potassium chloride for injection prior to dilution. Back then, it was common to find potassium chloride vials on nursing units in US hospitals, and the occasional mix-ups due to look-alike medication vials or mental slips led to disastrous outcomes. By 1987, ISMP had already convened a national meeting that helped influence USP and the US Food and Drug Administration (FDA) to require vials of concentrated potassium chloride for injection to have black caps and closures as well as warning statements to prevent mix-ups with other parenteral drugs. Nevertheless, potassium chloride vials remained on nursing units, and unsafe practices, such as not labeling syringes of potassium chloride intended for IV admixture preparation, continued to contribute to fatalities.
In 1995, ISMP sent a nationwide mailing to US hospitals that strongly recommended the removal of vials of concentrated potassium chloride for injection from patient care areas. Three years later, in the very first Sentinel Event Alert, The Joint Commission (TJC) asked hospitals to consider ISMP’s recommendation to not allow the vials outside of the pharmacy. By 2003, TJC required hospitals to remove concentrated potassium chloride and other concentrated electrolytes from all patient care units outside of the pharmacy in its inaugural National Patient Safety Goals. Since then, ISMP has been aware of only one case of accidental IV push of concentrated potassium chloride in the US in 2007 in a non-Joint Commission accredited hospital…until now.
ISMP recently received a report of an error in which concentrated potassium chloride was administered IV push to a patient during a cardiac arrest (code). In this hospital, concentrated potassium chloride vials were only stocked in the pharmacy, not on patient care units. Hands down, this is the most effective safeguard to prevent inadvertent IV administration of undiluted potassium chloride. Still, the event happened when a clinical pharmacist called the central pharmacy to ask staff to bring a vial of concentrated potassium chloride to a code he was attending. Through a series of miscommunications and incorrect assumptions, the drug was administered undiluted to the patient.
The Event
A 70-year-old intensive care unit (ICU) patient in isolation with a contagious infectious disease (not coronavirus disease 2019 [COVID-19]) experienced a cardiac arrest. To prevent unnecessary staff exposure to the infectious disease, the code was not announced overhead hospital-wide but only in the ICU. This resulted in a small team responding to the code—an experienced ICU intensivist, an experienced ICU pharmacist, and a nurse fellow and his preceptor (an experienced ICU nurse). In this hospital, the nursing fellowship program offered licensed nurses with some generalized experience the professional development necessary to become successful in a specialty field—in this case, ICU nursing.
During the code, the ICU intensivist verbally requested “potassium chloride 20 mEq IV.” The pharmacist, who was pulling and preparing the requested medications, assumed that the intensivist did not want to administer an infusion, which would have required an hour to administer. Instead, the pharmacist thought the intensivist had purposely ordered the drug to be administered undiluted via IV push, knowing it would stop the heart but assuming it was a new, unique treatment intended to save the patient during the code, as the intensivist had done previously during code situations with other medications. Furthermore, the pharmacist did not think to question the intensivist’s order because they had developed a very strong, trusting, working relationship. The pharmacist called the central pharmacy to request a vial of concentrated potassium chloride 20 mEq since the vials were not available on the unit or in the emergency cart as a safety precaution. The pharmacy delivered the vial to the patient’s room, without questioning why concentrated potassium chloride would be needed and assuming that the product would be diluted before administration.
The pharmacist asked the intensivist, “Do you still want to give potassium chloride 20 mEq IV?” while withdrawing the contents of the concentrated potassium chloride vial (20 mEq) into a syringe. When the intensivist said, “Yes,” the pharmacist handed the syringe to the nurse fellow, who administered the concentrated potassium chloride via IV push. Prior to administration, the nurse fellow did not verify with the intensivist that he would be administering undiluted potassium chloride 20 mEq IV push, nor did he verbally confirm administration of the drug afterwards. The patient developed asystole and was unable to be resuscitated. The error was discovered after the patient died when the intensivist asked how the potassium chloride had been administered.
Analysis of the Event
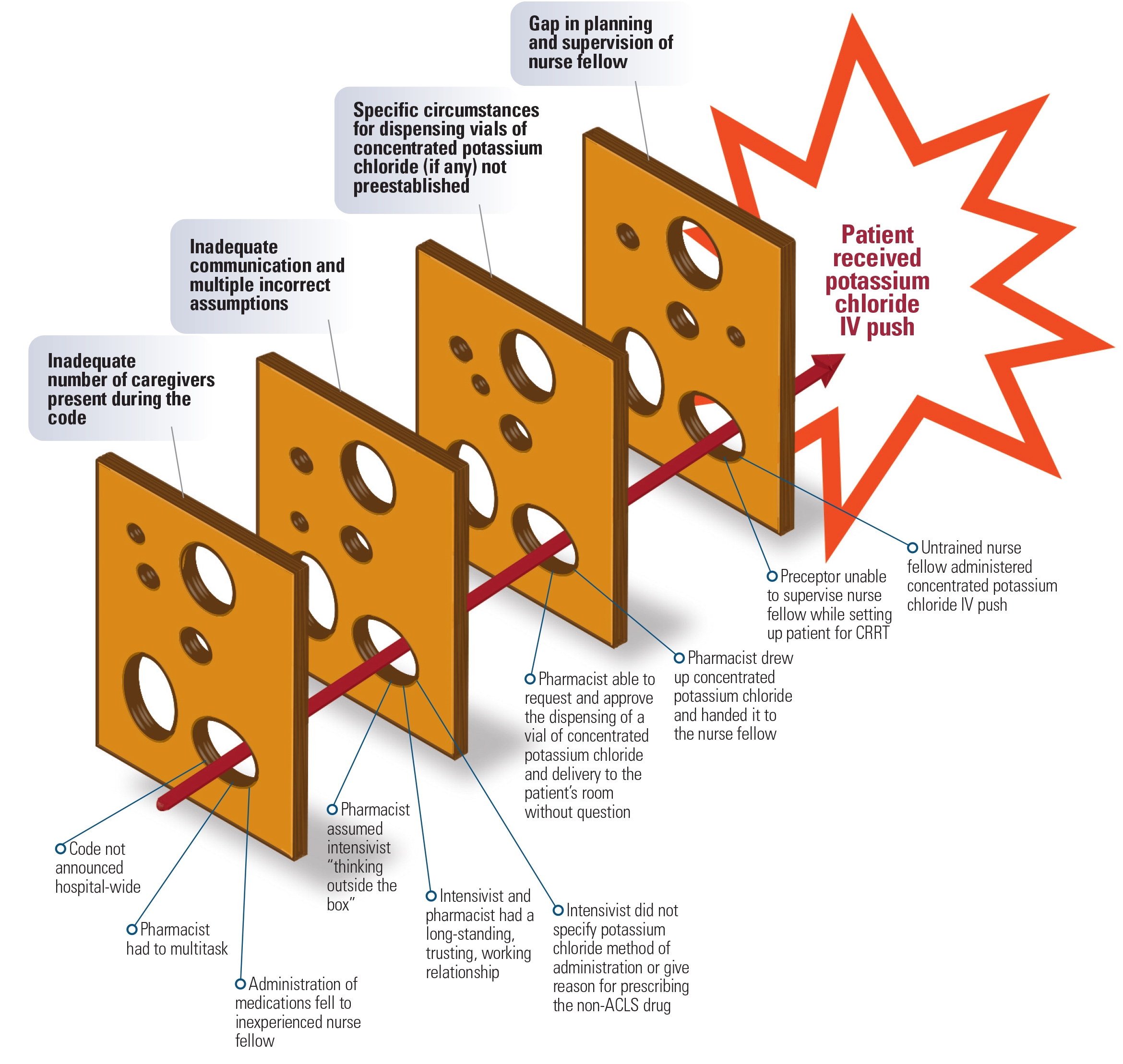
Storage of concentrated potassium chloride vials outside of the pharmacy did NOT contribute to this event, but removal of these vials from patient care units remains the primary risk-reduction strategy to prevent inadvertent IV administration of concentrated potassium chloride. However, the hospital identified four root causes of this event that might need to be addressed in US hospitals to prevent this specific type of error as well as other medication errors, particularly during codes. Figure 1 (below) provides a visual “Swiss cheese” illustration of the four root causes of the error.
Root Cause 1: An inadequate number of caregivers were present during the code because the code was not announced hospital-wide due to infection control concerns. Under normal code conditions, in addition to the intensivist, pharmacist, and fellow nurse and preceptor, the code team would have included, at a minimum, two experienced nurses to administer medications and defibrillate/monitor the patient’s heart rhythm; a respiratory therapist to maintain/monitor the patient’s airway; a scribe to document the code; a house supervisor to monitor the code and direct staff in and out of the room; and a safety monitor (runner) to assist in obtaining personal protective equipment (PPE) and other equipment for staff as needed. In this case, because the code team was small:
-
The pharmacist was asked to record the code, thus requiring him to document the code while preparing medications, distracting from his ability to focus on and validate the medications, doses, and drug preparation.
-
Administration of all medications fell to the inexperienced nurse fellow.
Additionally, due to a lack of clarity regarding how to call and conduct codes on contagious patients with infectious diseases other than COVID-19, the ICU care team enacted the COVID-19 code protocol to limit staff exposure to the patient’s highly contagious disease.
Root Cause 2: A lack of communication and incorrect assumptions among the code team led to the IV push administration of the concentrated potassium chloride. First, the intensivist did not communicate the reason for ordering potassium chloride, which is not an advanced cardiac life support (ACLS)-recommended medication. The intensivist did not share with the team that the patient’s potassium level had been low that morning, nor did she think it was necessary to clarify that the potassium chloride was to be administered diluted in a piggyback infusion—she assumed everyone knew that.
Next, the pharmacist did not clarify with the intensivist how she wanted the potassium chloride to be given (undiluted IV push or diluted infusion). Knowing that an infusion would require an hour, the pharmacist assumed the intensivist wanted to administer the drug faster. The pharmacist and intensivist had worked together in many code situations, and the pharmacist was used to the intensivist “thinking outside the box” in many previous dire situations. Although he knew that IV push administration of undiluted potassium chloride would stop the heart, the pharmacist had total confidence in the intensivist’s knowledge and skills and did not question what he assumed was a new and unique treatment. Also, when the pharmacist asked the intensivist, “Do you still want to give potassium chloride 20 mEq IV?” he did not specify “IV push.” Likewise, the nurse fellow did not verify the medication and how it was being administered with the intensivist prior to administration, as the nurse fellow had never attended a code and had not yet started his ACLS training.
Root Cause 3: Expectations had not been established to prohibit the dispensing of concentrated potassium chloride vials outside of the pharmacy without question. The pharmacy had not established reasonable criteria (certain circumstances, if any) for dispensing concentrated potassium chloride vials to a patient care unit (e.g., cardiac surgery). Thus, the pharmacist was able to request and approve the delivery of the vial to the patient’s room without an explanation regarding its use.
Root Cause 4: A gap in supervision led the nurse fellow to practice beyond the scope of his training by administering medications during a code. The nurse fellow was just a few weeks into his training, had never participated in a code, and had not yet received ACLS training. The gap in supervision occurred when the nurse fellow’s preceptor, an experienced ICU nurse, was busy getting the patient back on continuous renal replacement therapy (CRRT) during the code. Additionally, there was no formal description in the fellowship program regarding the nurse fellow’s role during code situations.
Safe Practice Recommendations: Consider the following recommendations to avoid medication errors, including with concentrated potassium chloride, during codes due to inadequate caregiver presence, miscommunications, lack of concentrated potassium chloride dispensing safeguards, and gaps in nurse fellow supervision.
Attendance
Announce codes overhead. Announce all codes overhead (or via a standardized beeper system) regardless of the patient’s isolation status to ensure adequate, trained caregivers are present to carry out critical roles during the code, without multitasking (e.g., scribe and preparing medications).
Establish guidelines to protect caregivers. Establish (or review) in-hospital resuscitation (code) guidelines and ensure they address caregiver protection from all highly infectious diseases. For example, some hospitals treat all patients as COVID-19 positive given the prevalence of asymptomatic disease in the population.
Keep those not providing direct care outside the isolation room. Minimize the code team who enters an isolation room to the smallest number of ACLS caregivers possible, requiring support staff (e.g., scribe, runner, house supervisor) to remain in the hallway outside the room, along with the full code cart. (An “immediate use drug bag/box” and defibrillator can be passed to caregivers in the room, along with other drugs and equipment as required.) Include an adequate supply of PPE near the code cart and require all caregivers who enter the isolation room to don the PPE.
Communication
Specify the route and method of administration. The intensivist/prescriber in charge of the code should specify the route and method of administration for all medication orders, clearly delineating between IV push and IV infusions.
Specify non-ACLS medications. If time permits, the intensivist/prescriber in charge of the code should let the code team know when they order a non-ACLS medication and include a brief indication/reason.
Verify the medication. The caregivers preparing and administering each medication should repeat back the entire medication order (drug, dose, route, method of administration [including IV push or IV infusion, as applicable]) for confirmation during preparation and prior to administration. The entire medication order should again be repeated back after administration, so the intensivist/prescriber knows what has just been administered.
Empower caregivers to ask for clarification. Create a safe environment and teach and empower caregivers to clarify questionable or incomplete medication orders. Do not make assumptions about a questionable or incomplete order, even in the presence of a strong and trusting working relationship.
Practice communication. Hold mock code simulations, including ones in isolation scenarios, to reinforce the closed loop communication required among the team members and to acknowledge the challenges faced in this unique situation.
Evaluate communication post-code. Specifically evaluate the completeness and clarity of communication among the code team during the post-code debriefing. If applicable, add to your post-code debriefing form, “How was our communication during the code?” Plan and implement improvements as necessary.
Concentrated Potassium Chloride Safeguards
Dispense vials per preestablished criteria. Do not take injectable potassium chloride safety for granted, even after years of no reported events. Clearly describe any specific circumstances when concentrated potassium chloride vials may be dispensed from the pharmacy, and establish safeguards for those circumstances to avoid errors. (In the hospital where this event happened, there are no circumstances where dispensing of concentrated potassium chloride vials is now allowed.) In the pharmacy, ask questions to make sure that any request to dispense the vials clearly falls within the preestablished criteria, and inquire whether the required safeguards are in place. If the request does not match preestablished criteria, question it. Remember, potassium chloride is not a life-saving medication. If a potassium chloride infusion is not available in a premixed bag, as a general rule, it should be prepared in the pharmacy where safety checks are in place.
Role of Nurse Fellows
Observation and shadowing. Nurse fellows (and other caregivers) who have not completed ACLS training should only be allowed to observe during a code. After ACLS training, the nurse fellow and preceptor should function as one, with the fellow shadowing the preceptor during the code, without taking a primary or separate role during the code. Preceptors should also receive specific guidance in advance of any assignment regarding any limitations of the nurse fellow’s role.
Conclusion
Let this error serve as a call to action for code teams across the nation to evaluate their systems and processes to determine if any of these risk factors could be present in their facilities. One of the benefits of learning from the mistakes of others is realizing you could make the same errors. Please implement the above recommendations to avoid a repeat of those failures. As the familiar saying tells us, “An ounce of prevention is worth a pound of cure.” We also hope you will incorporate this error story, analysis, recommendations, and the results of your internal evaluation into your ACLS training scenarios and practitioner competencies. Lastly, please remember that second victim support should be considered and provided after any event that causes significant patient harm.
Access this Free Resource
You must be logged in to view and download this document.
